Products
Services
February 2, 2016
This attestation guide is designed to help you through the attestation process for the CMS – EHR Incentive Program and is specific to Medicare. If you plan to attest for Medicaid please contact your state Medicaid office for further details.
Below is an example exclusion form created by ChartLogic. You can download this form here.
CMS has an Attestation Calculator designed to assist you with the process. Click here to launch.
https://ehrincentives.cms.gov/hitech/login.action
Read any system announcements and schedule your attestation accordingly. Click Continue, when ready.
Carefully review the About This Site information. Click Continue, when ready.
Carefully read the information on the Warning page. Check the box to indicate that you are aware of the statements on this page and click Continue, when ready.
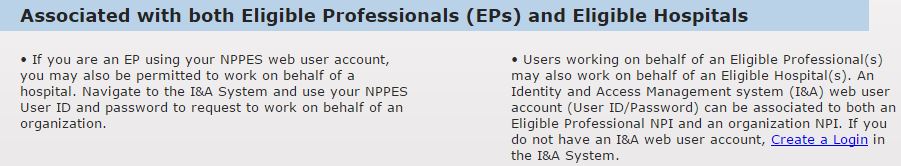
The next page will allow you to login or create an NPPES login. If you are having issues with your User ID/Password and are unable to log in, please contact the CMS EHR Incentive Program Information Center: 888-734-6433 / TTY: 888-734-6563
Eligible Physicians (EP) or users working on behalf of an EP can create a NPPES login by following the instructions below:
When ready, click Attestation to begin the attestation process.
This will take you to the Medicare Attestation Selection page. Here you’ll see previous attestation years to verify your current program year. When ready, click Attest on the current year.
This will take you to the main Attestation page. From here you’ll click Attestation Information to get started.
Verify that the Certification number is correct and select a valid date range for the reporting period. When ready, Click Save & Continue.
The next page will go over measures required by CMS to meet meaningful use. At the bottom of this page, you’ll need to select the public health options you’ll be attesting for. You may need to claim an exclusion if your public health agency does not accept public health reporting data, or you don’t meet the criteria to report on these measures.
If claiming an exclusion on any of the Public Health Reporting Measures, you’ll be required by CMS to report on or also claim an exclusion on the remaining measures listed below.
*If you claim an exclusion on any measure, CMS also wants exclusion information for the remaining measures.
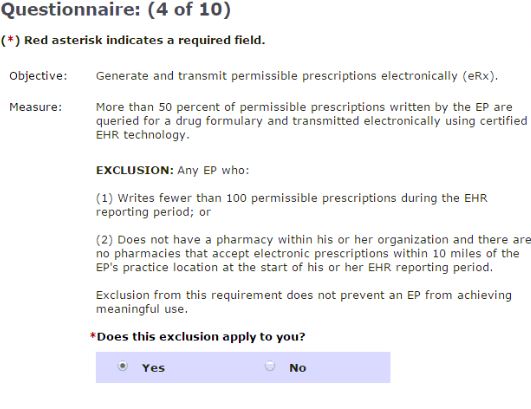
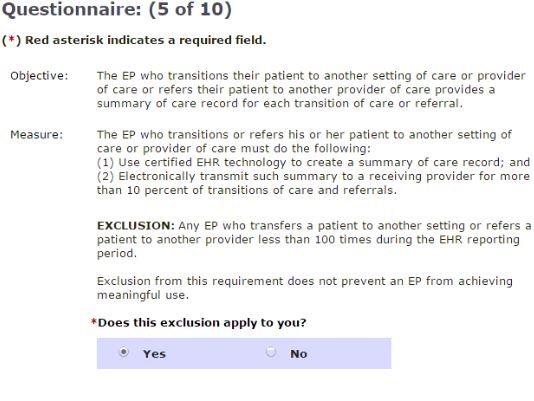
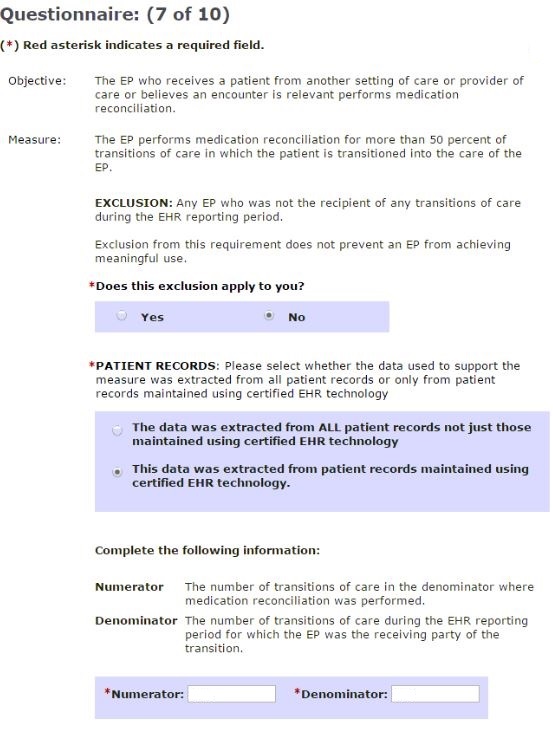
Not all measures have an available exclusion. For measures with an available exclusion, you will need to specify if the exclusion applies to the provider. You will need to do this for each provider and each excluded measure, per objective. If the exclusion applies, click Yes when asked “Does this exclusion apply to you?” and document the reasons as to why you are excluded from this measure. Use the Meaningful Use Exclusion Document available here.
If you do not qualify for an exclusion, you’ll click No when asked, “Does this exclusion apply to you?” You’ll then have to record a numerator and denominator from the 2015 Meaningful Use Report to satisfy the measure.
Keep copies of all exclusion documentation, as this will assist with any future audits.
This measure is asking for the Security Risk Analysis that is dated during the reporting period. HealthIT.gov offers a free tool to assist in completing this measure. Click here to launch the tool.
Indicate whether this exclusion applies to you or not. If not:
Indicate whether this exclusion applies to you or not. If not:
Indicate whether this exclusion applies to you or not. If not:
Indicate whether this exclusion applies to you or not. If not:
 Indicate whether this exclusion applies to you or not. If not:
Indicate whether this exclusion applies to you or not. If not:
Indicate whether this exclusion applies to you or not. If not:
Indicate whether this exclusion applies to you or not. If not:
 Indicate whether this exclusion applies to you or not. If not:
Indicate whether this exclusion applies to you or not. If not:
Indicate whether this exclusion applies to you or not. If not:
Measures 10A, 10B, and 10C will require your state’s Department of Health (DOH) to have the ability to accept this information. Please visit your state’s DOH website to verify the capability to report on Immunization registry, Syndromic Surveillance, or other specialized registries.
This will bring you to Reporting Clinical Quality Measures. For example, ChartLogic software is certified for nine CQM measures. You’ll click Option 2 to select the correct CQM measures.
You’ll now be on the CQM Selection page. Read the Instructions listed below and select the nine CQM measures. Click Save & Continue.
All nine CQM Measures are required to be reported on for successful attestation. To obtain CQM data please contact your EHR/EMR vendor.
| Measure ID | Measure Title | CMS Domain |
| CMS138 | Preventative Care and Screening: Tobacco | Pop/Pub Health |
| CMS153 | Chlamydia Screen for Women | Pop/Pub Health |
| CMS117 | Childhood Immunization Status | Pop/Pub Health |
| CMS166 | Use of Imaging Studies for Low Back Pain | Efficient use of Healthcare Resources |
| CMS165 | Controlling High Blood Pressure | Clinical Process |
| CMS126 | Use of Appropriate Medication for Asthma | Clinical Process |
| CMS127 | Pneumonia Vaccinations for the Elderly | Clinical Process |
| CMS123 | Diabetes Foot Exam | Clinical Process |
| CMS65 | Hypertension: Improve in Blood Pressure | Clinical Process |
At this point in the attestation, you are ready to record CQM data.
On the next page you will be asked to ensure that this information is correct. Once you review this data for accuracy, you will have the option to submit.
After submitting your attestation, we suggest printing the acceptance receipt and keep all reports, exclusions and supporting documentation for this attestation period. This information will be required as proof of your answers in the event of an audit.
If you have any questions related to attestation or would like to purchase attestation assistance, please contact ChartLogic: 800-838-5899 or contact us.